March 10, 2025
Should You See an Oncologist if You’re Diagnosed with Melanoma?

Melanoma is not the most common type of skin cancer, but it is the most serious. Melanoma tends to be aggressive which means it grows and spreads quickly. However, when detected and treated early, melanoma is usually curable.
If melanoma was found on your skin, it was likely diagnosed and possibly treated by a dermatologist. But is that enough? While dermatologists can often remove the affected area through surgery, it may be wise to meet with an oncologist after the procedure, even if the cancer was at an early stage, to see if more treatment can reduce the likelihood of melanoma recurrence. If your melanoma is diagnosed at an advanced stage, you will most likely need more than surgery to treat it. An oncologist will meet with you to discuss a cancer treatment plan.
Let’s take a deeper look at what melanoma is and how both a dermatologist and an oncologist may play a role in the treatment process.
What is Melanoma?
Melanoma is an aggressive type of skin cancer that occurs when melanocytes, the cells responsible for skin pigmentation, begin to grow uncontrollably. These cells are primarily located at the bottom of the epidermis, the outer layer of the skin.
While melanoma can develop anywhere, it’s most frequently found on skin that was exposed to ultraviolet (UV) light from the sun and tanning beds. The most commonly affected areas include the arms, back, chest, face, and legs. Most melanomas start in normal skin, however, some begin in existing moles.
Melanoma is categorized into five stages, ranging from 0 to IV, based on how deeply the cancer has penetrated the skin and whether it has spread to other areas. Stage 0 melanoma is localized and non-invasive, while stage IV melanoma means the cancer has spread (metastasized) to distant parts of the body.
Due to its aggressive nature, early detection can be life saving!
The Role of a Dermatologist in Early Melanoma Treatment
If you notice an unusual spot or growth on your skin, it's important to have it examined by a dermatologist as soon as possible. You should also make sure you’re going once a year to have your skin evaluated by your primary care doctor or a dermatologist to look for new developments on the skin that may be a cause for concern.
Learn more about the signs and symptoms of melanoma and other skin cancers.
If an area of concern is small and appears to be skin cancer, it will be thoroughly examined and a biopsy will be performed. This simple procedure can usually be done in the doctor’s office. A skin biopsy is the only way to confirm whether you have skin cancer.
If the biopsy results confirm early-stage melanoma, the dermatologist may schedule you for another outpatient procedure called a wide excision. This involves numbing the area and surgically removing a larger margin of skin surrounding the melanoma to be sure all of the cancer cells are removed.
However, if the melanoma is located in a hard-to-reach or sensitive area, or if it has progressed to a more advanced stage, you may be referred to a surgical oncologist for further testing, a more complex surgery, and additional skin cancer treatment.
If your melanoma was detected early and surgically removed by the dermatologist, you may be put on observation. This will involve regular visits to the dermatologist to check for signs of new melanoma development.
When Is it Time to See an Oncologist for Melanoma?
Melanomas that have grown deeper into the skin or have started to spread usually require treatment from an oncologist. The oncologist will likely begin with a sentinel lymph node biopsy (SLNB) to check for cancer in nearby lymph nodes.
If the lymph nodes show no sign of cancer, further treatment may not be necessary. However, if cancer cells are found in the lymph nodes, a lymph node dissection—surgical removal of the cancerous lymph nodes—might be recommended along with other treatments to be sure any cancer cells that have traveled through the lymph system to other areas of the body are treated.
For some Stage II, III, and IV melanomas, additional treatments are needed, which include:
Immunotherapy: This treatment boosts the immune system's ability to fight cancer. In the case of melanoma, immune checkpoint inhibitors may be used after surgery if cancer has spread to the lymph nodes or other parts of the body.
Targeted therapy: Certain melanomas with specific genetic mutations may respond to medications designed to precisely target them. Your oncologist will determine if there are any genetic mutations causing the cancer to grow by running biomarker tests. The right targeted therapies are selected for each patient based on the biomarker test results.
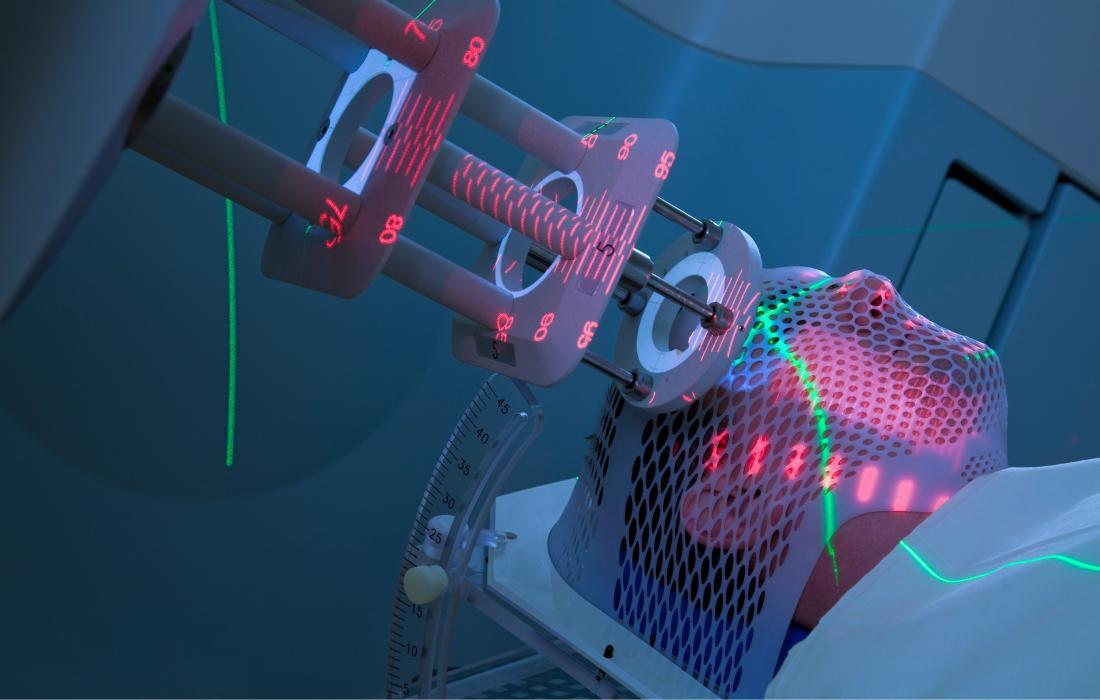
Radiation therapy: External beam radiation therapy may be used after surgery to kill remaining cancer cells or in cases where surgery is not an option. Additionally, topical high-dose-rate (HDR) radiation can be applied by placing the radiation source close to the skin for short periods.
Chemotherapy: Chemotherapy medications may be given when advanced melanomas do not respond to immunotherapy or targeted therapy.
The oncologist and cancer care team can work with your dermatologist to create a comprehensive skin cancer treatment plan tailored to your needs. For some patients, this may also include clinical trials, providing access to advanced treatments.
Melanoma Survival Rates: The Earlier the Better
Fortunately, patients diagnosed with melanoma now have a better outlook thanks to advances in treatment. The 5-year survival rates for melanoma patients vary by stage:
Localized (Stage 0 and I): Approximately 99%-100% survive for at least five years if the cancer has not spread beyond its original location.
Regional (Stage II and III): Approximately 75% or more of the patients survive for at least five years if the cancer has spread to nearby structures or lymph nodes.
Distant (Stage IV): About 35% of metastatic melanoma patients survive for five years or more.
As you can see, detecting melanoma early greatly improves the likelihood of a positive prognosis and successful recovery.
How to Look for Skin Cancer
Early detection and diagnosis of skin cancer significantly improves the chances of successful treatment outcomes. In addition to annual exams, the American Cancer Society recommends conducting regular self-exams, looking for new spots and any changes in the shape, size, or color of existing ones. Pay attention to any "ugly ducklings" on your skin or any mark that stands out or looks different from the others.
The following ABCDE rule is a helpful guide for identifying potential melanomas:
A for Asymmetry: One half of the mole or mark does not match the other half
B for Border: The edges are irregular, jagged, blurry, or notched
C for Color: The mole has a non-uniform color, exhibiting different shades of black or brown or red, white, pink, or blue
D for Diameter: The mark is more than ¼ inch in diameter (about the size of a pencil eraser)
E for Evolving: The mole is changing in color or shape or is growing
Regularly checking your skin is easy! Don’t forget to check your back and the bottoms of your feet!
While not every skin cancer follows these rules, many do. If you notice any suspicious spots on your skin, have them promptly examined by a dermatologist. This is especially important for aggressive types of melanoma, like amelanotic melanoma, which can be harder to detect because it lacks the typical dark pigmentation. Delaying a visit to the dermatologist could allow the cancer to progress to a more advanced stage, making treatment more difficult and potentially reducing treatment options
RELATED READ:
What is the Difference Between Precancerous Skin Growths and Skin Cancer?

Melanoma Treatment in Brevard County, Florida
If your dermatologist diagnosed you with melanoma, talk to them about seeing an oncologist as well. At Cancer Care Centers of Brevard, our team of skin cancer specialists will work together to determine the best treatment options for your melanoma. We have multiple locations in Florida, including Melbourne, Merritt Island, Palm Bay, and Rockledge. Schedule a consultation with one of our experienced oncologists today.
Categories: Skin Cancer